Testosterone Series Part 4. Let’s Talk About Nebido, Sustanon and Enantate


This series has been a long time coming as my time gets limited and other interests drive my focus elsewhere but TRT is still one of the things I most enjoy doing. The idea of this blog is to give a more medically based opinion on the 3 commonest injectables used in the UK; my experience with it and my patients’ experience with it including labs.
Firstly, I’d like to touch upon the fact that this blog is not referring to testosterone cycles- what you normally see in forums- that focus more on body building. The focus is on sub-optimal testosterone levels being brought back up to optimal levels.
The 3 commonest injectables that I use at my practice and their various quirks are summarised below:
commonest due to price.
Comes in ampoule only. If you are getting it online in a vial, its not from a UK pharmacy.
Claims to be sustained release- hence called susta-non due to having 4 different esters (or carrier molecules). Each ester releases the testosterone at a different time and hence you get a more staggered release pattern where the peaks and troughs are more stable.
Single 1ml shot lasts 2.5 to 3 weeks. It can be given in divided doses.
Main disadvantage- carrier oil is peanut oil and benzyl alcohol. This is becoming a problem I’m seeing more and more of as its giving rise to side effects which I don’t get with other injectables. Most people with mild intolerances generally don’t even know they cannot handle peanut oil. When given in such large doses (1ml into the muscle), it can cause pain and local inflammation that lasts much longer than expected. As part of my practice is gut dysbiosis where I see a lot of food intolerances, I recognised this very early on. If this is your experience too, try changing to the other injectables or use creams.
The average response I get when I ask about peanuts is that my patients love it! Do keep an open mind about intolerances- just because you love it does not mean that you can handle it. Look out for other symptoms of intolerances like joint pains, rashes, headaches, flu-like symptoms etc. You may get none, or all of them.
This is the most similar to Cypionate that many people read about in forums. Cypionate is available in the US and some other countries but not in the UK. Its what I would put my patients on who need continuity of care from the US.
Its quite a bit more expensive that sustanon- stupidly more in fact. I don’t know why!
Comes in ampoule only. If you are getting it online in a vial, its not from a UK pharmacy. The ones in vials are considerably cheaper- according to google and from what some of my patients tell me- but we practitioners will never advocate it. Its just not worth it to me.
Is given in the same way as Sustanon- either single shot that last 2-3 weeks or in divided doses.
Carrier oil here is castor oil which is less allergenic (apparently) and benzyl benzoate.
I personally have never had a complaint with this so suspect that it probably is less allergenic.
If the price point of this and sustanon were the same, I would prefer using this.
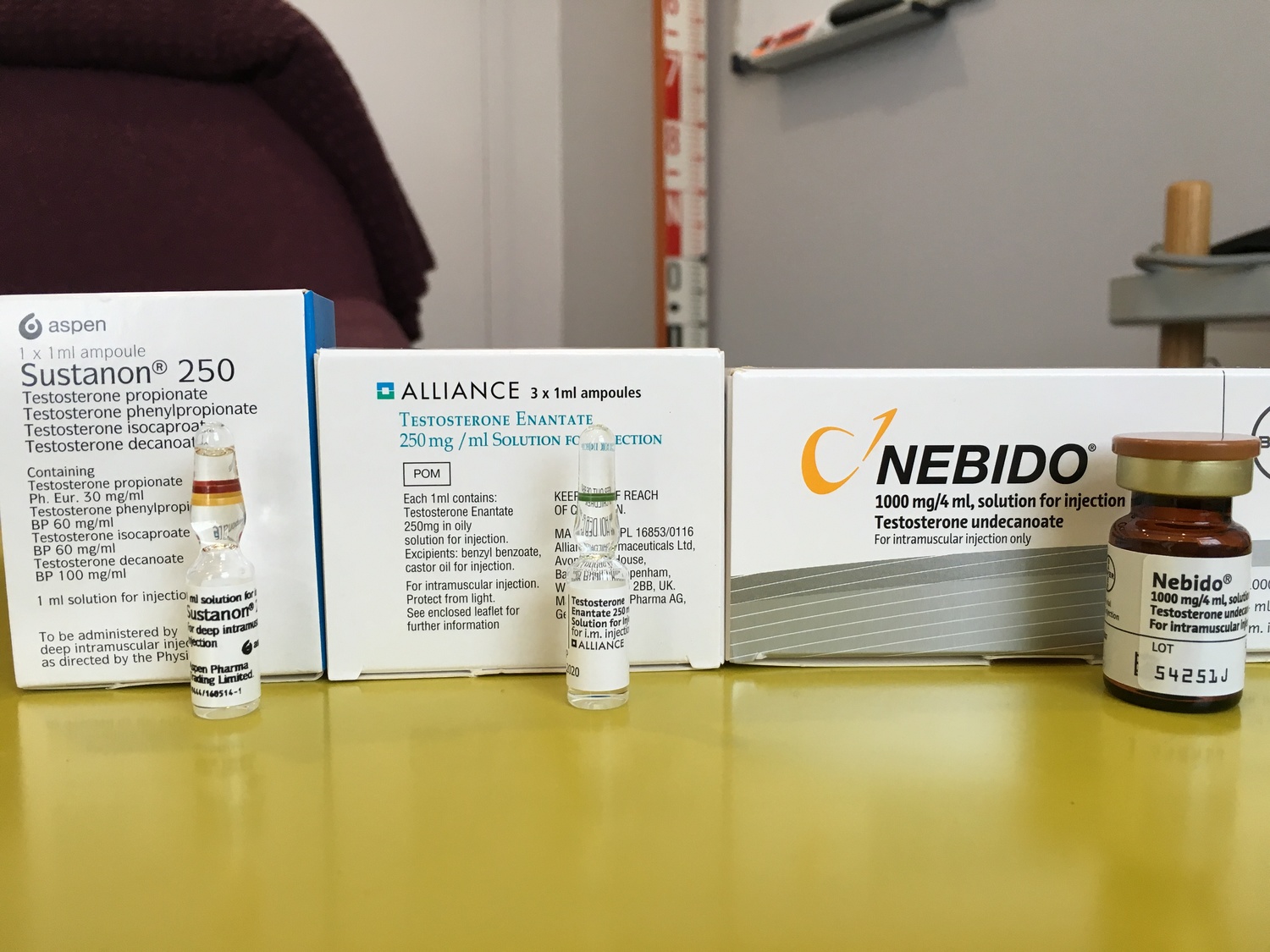
TAKEN AT OUR CLINIC
This can hurt but its usually due to the volume of product injected into a small area. I occasionally inject it either in both buttock cheeks especially in very slim patients, or change directions still with the same entry point to spread things out a little.
This comes in a vial.
Carrier oil here is refined castor oil which is less allergenic (apparently) and benzyl benzoate.
I’m not a huge fan of Nebido but it has its place. I personally prefer it for patients who have completed their family (for potential fertility implications), travel a lot, have compliance issues or similar reasons.
This always suppresses your pituitary hormones which means that the negative feedback generated will block your own production of testosterone.
On a practical level, a lot of people don’t mind it and are happy to put up with some testicular shrinkage- as long as everything is being monitored regularly.
Others freak out a little when their pituitary levels of LH comes back as close to nonexistent. They can either opt for a different option or start on a HCG protocol (Human Chorionic Gonadotropin) to stimulate their own production of testosterone alongside testosterone. Its a protocol used a lot in the US and quite many of my American patients request the same continuity of care as it works well for them.
There are also a small number who really feel the peak- not in a good way. Optimal levels of testosterone usually makes you calmer and less anxious but too much or too little can give rise to similar symptoms paradoxically when it comes to moods and aggression.
Bioidentical topical creams from Compounding Pharmacies– I use these a lot and my patients love them (mostly). They are much easier to use compared to the gels available on the NHS (messy, too large a volume and sometimes does not give the blood picture expected which may point to user inconsistency in application).
My topicals come in 3 forms- creams, gels or liposomal gel. I have so far only ever ordered the liposomal gel as its absorbability is far superior at no extra cost.
As these are bespoke, there is a period of trial and error until you find the right dose after which, we simply make the cream in said dose for each patient.
Its more physiological with everyday application and so mimics the body’s own production more closely. This also translate into less pituitary suppression.
Disadvantage- some people perceive creams to be less effective (not true). Some don’t like having to apply a cream everyday.
I hope that this article will help you gain an idea of what is available legally via a pharmacy in this country and to be able to tell the difference between what may or may not suit you. Or why you may be reacting to something others don’t have a problem with. As with most things medical, its not quite that simple but getting the right balance is possible and certainly achievable.
If you’d like to speak to us about TRT, please don’t hesitate to call our friendly admin team on 020 7096 5475. Alternatively, you can book an appointment online by clicking the button below.